










 Official publication of the Czech Society of Ultrasound in Obstetrics and Gynecology.
Official publication of the Czech Society of Ultrasound in Obstetrics and Gynecology.

Placental abruption is a potentially life-threatening obstetric complication, often associated with hypertensive disorders of pregnancy. While its occurrence in the context of preeclampsia is well-documented, it is uncommon for placental abruption to serve as the initial clinical manifestation. We report the case of a 23-year-old primigravida at 30 weeks of gestation who presented with abruptio placentae and was subsequently diagnosed with severe preeclampsia. Intraoperative findings revealed a Couvelaire uterus, a rare consequence of placental abruption characterized by extravasation of blood into the myometrium. Prompt cesarean delivery and conservative management resulted in favorable maternal and neonatal outcomes. This case underscores the importance of recognizing atypical presentations of hypertensive disorders during pregnancy and the critical role of timely intervention.
Preeclampsia remains a major contributor to maternal and perinatal morbidity and mortality worldwide, affecting approximately 5-8% of pregnancies. Classically defined by the onset of hypertension and proteinuria after 20 weeks of gestation, preeclampsia encompasses a spectrum of severity and clinical manifestations. While most cases develop gradually and are identified through routine antenatal monitoring, atypical presentations pose significant diagnostic and management challenges. The pathophysiology of preeclampsia is commonly explained by a two-stage model. The first stage involves abnormal placentation due to inadequate trophoblastic invasion and failed remodeling of the spiral arteries, leading to placental ischemia. The second stage reflects the maternal systemic response to placental-derived factors, resulting in endothelial dysfunction and clinical features such as hypertension and proteinuria (1,2). Placental abruption, defined as the premature separation of a normally implanted placenta, is a serious obstetric emergency with a prevalence of 0.3–1%. It occurs more frequently in women with hypertensive disorders and can result in severe maternal and fetal morbidity and mortality. The Couvelaire uterus, although rare, represents a dramatic sequela characterized by blood infiltration into the myometrium. This report highlights an unusual sequence in which placental abruption revealed previously undiagnosed severe preeclampsia, emphasizing the need for clinical vigilance and timely surgical intervention (3).
A 23-year-old primigravida at 30 weeks of gestation, with no prior medical or obstetric history, presented with a severe frontal headache, lower abdominal pain, and bilateral lower limb edema. Her blood pressure was 180/110 mmHg. Shortly after admission, the patient developed profuse vaginal bleeding. On clinical examination and ultrasound, a diagnosis of severe placental abruption was established. The patient was in hypovolemic shock and exhibited signs of pitting edema.
Laboratory investigations revealed: hemoglobin 110 g/L, platelet count 142 × 10^9/L, AST 250 U/L, ALT 98 U/L, LDH 751 U/L, and serum albumin 25 g/L. Proteinuria was 1600 mg/g. An emergency cesarean section was performed under general anesthesia. A female neonate weighing 1440 g was delivered with APGAR scores of 5, 5, and 7 at 1, 5, and 10 minutes, respectively, and was admitted to the neonatal intensive care unit. Intraoperatively, a Couvelaire uterus was observed with widespread ecchymosis and intramural hemorrhage. The uterus was preserved, and hemostasis was achieved without requiring hysterectomy. Postoperatively, the patient developed generalized edema and marked hypoalbuminemia (20 g/L), necessitating intensive care and transfusion of fresh frozen plasma. After stabilization, the patient was discharged on the seventh postpartum day. The neonate remained hospitalized for four weeks and was discharged in stable condition.
This case highlights an uncommon clinical scenario in which severe preeclampsia presented initially with placental abruption. Although these two obstetric complications frequently coexist, the occurrence of abruption as the sentinel manifestation of preeclampsia is rare and can delay appropriate diagnosis and management. In a large retrospective cohort study, hypertensive disorders of pregnancy as a principal risk factor for placental abruption, with hypertension typically diagnosed before or simultaneously with the abruption event (4). The atypical chronological sequence observed in this case, where abruption preceded any clinical or laboratory indicators of preeclampsia, emphasizes the need for heightened clinical vigilance, especially in emergent obstetric settings. A particularly significant feature in this case was the development of a Couvelaire uterus, a rare but severe complication of placental abruption characterized by extensive hemorrhagic infiltration of the uterine myometrium and serosa. Traditionally, this condition was considered an indication for per partum hysterectomy due to the presumed inability of the uterus to contract effectively and control bleeding. However, emerging evidence from recent case series supports the feasibility of conservative management, including uterine preservation, in hemodynamically stable patients, provided that timely surgical intervention and multidisciplinary care are available (5,6,7,8). The successful avoidance of hysterectomy in this patient contributes to the limited but growing body of literature advocating for fertility-sparing strategies in appropriately selected cases. This report also underscores the critical importance of early recognition of atypical presentations of hypertensive disorders in pregnancy. In the absence of classic symptoms such as sustained hypertension or proteinuria, ancillary clinical signs, laboratory parameters, and the presence of obstetric complications such as abruption must raise suspicion for underlying preeclampsia. Prompt diagnosis and coordinated multidisciplinary management are essential to reduce morbidity and mortality for both mother and fetus. This case thereby reinforces the clinical imperative to consider preeclampsia in the differential diagnosis of unexplained placental abruption and supports an individualized approach to the management of the Couvelaire uterus. Placental abruption is associated with preterm delivery. In cases where patients present to labor and delivery with signs such as vaginal bleeding, abdominal pain, prompt assessment and intervention are crucial. Although clinical management can be complicated by fetal compromise and maternal coagulopathy, early identification of disseminated intravascular coagulation (DIC), appropriate use of blood products, and timely delivery are key components of effective care. Evidence-based guidance for managing placental abruption at later gestational ages, with rapid and coordinated care, can significantly improve neonatal and maternal outcomes (3).
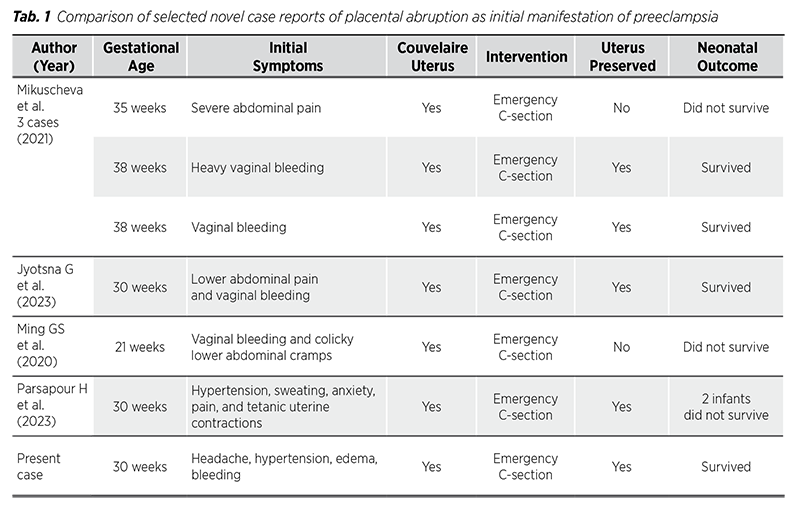
Table 1 presents a comparative summary of similar novel published case reports that document placental abruption as the initial manifestation of preeclampsia, highlighting differences in presentation, intervention, and outcomes.
This case emphasizes the importance of maintaining a high index of suspicion for preeclampsia in patients presenting with placental abruption, even in the absence of a prior diagnosis. It also illustrates the feasibility of conservative surgical management in cases of Couvelaire uterus. Early recognition, coordinated multidisciplinary care, and prompt surgical intervention are key to improving maternal and fetal outcomes. Further studies are necessary to refine diagnostic strategies and treatment protocols for atypical presentations of preeclampsia.
Conflicts of Interest: The authors declare no conflict of interest.
Funding: None.