










 Official publication of the Czech Society of Ultrasound in Obstetrics and Gynecology.
Official publication of the Czech Society of Ultrasound in Obstetrics and Gynecology.

Multiple pregnancies carry increased risks for both mother and fetus, such as a higher incidence of morphological and chromosomal abnormalities. Screening for aneuploidy in multiple pregnancies is currently limited. Multifetal reduction is one of the possible ways to manage multiple pregnancies that would otherwise not progress or be terminated at the request of a pregnant woman within the legal time limit. A pregnant woman should have the opportunity to be informed whether the remaining fetus bears a chromosomal abnormality. Given the increased risk of aneuploidy in multifetal pregnancies and given the relatively low risk of diagnostic testing in the context of the overall management of multifetal pregnancies, analysis of an amniotic fluid sample at a sixteenth week of pregnancy is a possible alternative.
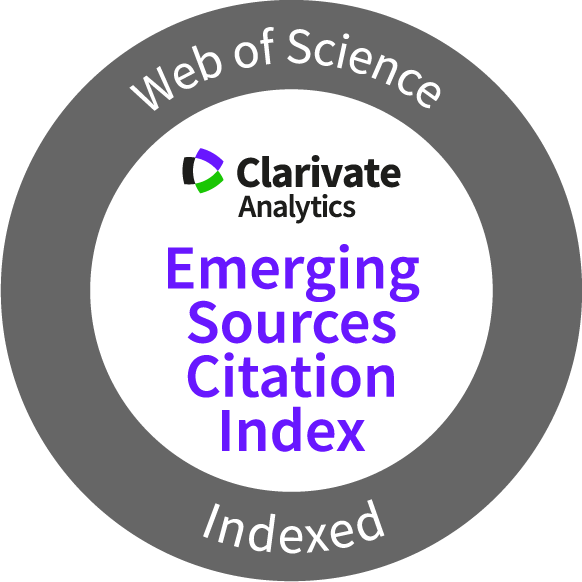
Humans are monotocous (producing a single offspring at birth), and the uterus is biologically adapted for one fetus. Multiple pregnancy is a relatively rare situation with an incidence of 1 in 85 births (i.e., 11.7 twins per 1,000 births) (1,2). Twin pregnancy causes a higher risk for the mother (preeclampsia, gestational diabetes, anemia, operative delivery, postpartum hemorrhage) and fetuses (increased incidence of congenital, morphological, and chromosomal defects). Simultaneously, with the occurrence of morphological defects, there is a higher incidence of chromosomal defects (3). Twin pregnancies show higher incidences of prematurity (4), cerebral palsy (5), and fetal growth restriction (6). The resulting higher maternal and newborn morbidity and mortality burden the health system with significantly higher healthcare costs (7,8). This situation is clearly visible in the graphs comparing the perinatal mortality of singleton and twin pregnancies in the Czech Republic between 2004 and 2021 (Graphs 1 and 2).
In addition to the medical complications of a twin pregnancy, little attention is paid to the quality of life of the entire family, which must adapt its functioning to the birth and simultaneous care of multiple offspring, where parents of multiples experience heightened symptoms of depression, anxiety, and parenting stress (9).
Multifetal reduction (MFR) consists of reducing the number of developing fetuses to reduce the risks of pregnancy (10). MFR has been proven to reduce risks for the preserved fetus, including the risks of premature birth, low birth weight, and spontaneous abortion (11). There is also a demonstrable benefit for the mother, in which MFR enables a safer and more comfortable pregnancy with a lower risk of preeclampsia, birth complications, and operative delivery (12). The effect on the psyche and quality of life of the pregnant woman is also significant (13,14). The multifetal reduction must be distinguished from so-called selective termination, which targets the reduction of the fetus affected by a genetic or morphological defect (15).
Multifetal reduction has been performed since the 1980s. It was developed as a reaction to the iatrogenic consequences of assisted reproduction when a higher number of embryos is transferred with the aim of increasing the success rate of in vitro fertilization (IVF) (16). Today, with single embryo transfer being promoted in IVF programs, the proportion of multiple pregnancies due to embryo transfer is no longer significant (17). It has been reported that an important source of multiple pregnancies is poly- ovulation due to the administration of clomiphene citrate (18), whereas in the Czech Republic, there is no direct data from which we could verify this statement.
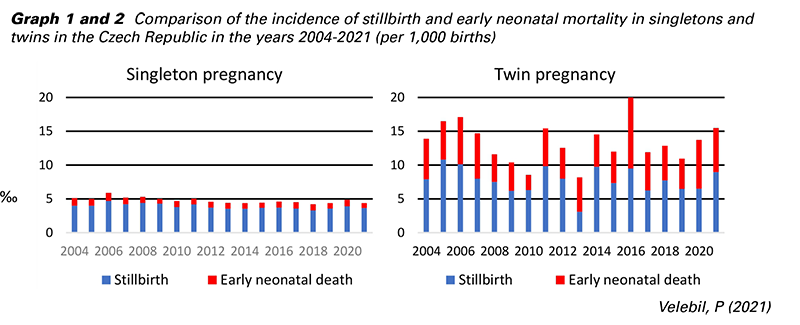
In the Czech Republic, since 2010, it has been possible to continuously reduce the incidence of multiple pregnancies by promoting single embryo transfer and reducing the overuse of clomiphene citrate. While 2010 had the highest number of twins born in history (21.3 per 1,000 births), in 2021, 11 years later, only 12.7 twins per 1,000 births were registered (Graph 3). This incidence (1 in 80 births) roughly corresponds to the situation before the introduction of assisted reproduction methods, i.e., from the time when ovulation induction or embryo transfer methods were not used (1). Therefore, the influence of iatrogenic poly-ovulation after the administration of clomiphene citrate is no longer significant and that a kind of plateau, which has currently been reached, will no longer decrease significantly in the future.
We have performed multifetal reductions since the beginning of the 1990s. In the years 2005–2021, we performed a total of 342 two-to-one reductions, which corresponds to an annual average of 20.12 multifetal reductions (min 13, max 28). These reductions mainly concerned women who turned to us in situations where they would otherwise have exercised their right to terminate their pregnancy in the first trimester without giving any reasons. Multifetal reduction is therefore an intervention that allows a pregnancy to continue with one fetus and reduces the risks of complications from a twin pregnancy.
MFR itself is a complex and emotionally demanding decision. Pregnant women are consulted in a nondirective manner and introduced to objective possibilities, alternatives, and risks. The resulting decision is fully within the pregnant woman’s ability, who has enough time to re-think and ask additional questions.
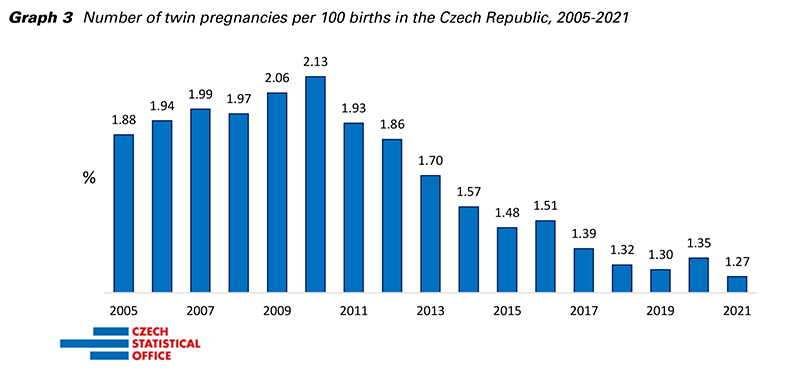
Graph 4 and 5 show the results of our retrospective observational study from 2011-2016. By comparing groups of women with twin pregnancies and reduced twin pregnancies from the same time period, we concluded that in the group with reduction, fewer premature newborns and newborns with lower birth weight were born. Furthermore, the incidence of cesarean delivery was significantly lower, and above all, delivery by unplanned emergency cesarean section. These data are in agreement with the published literature (11,12).
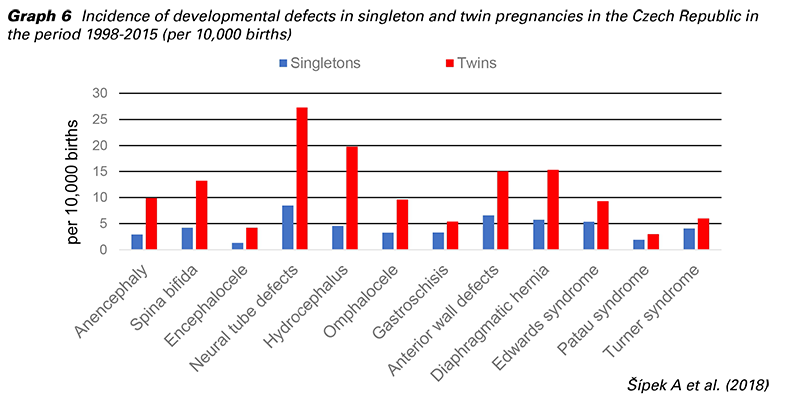
Compared to singletons, twins have a higher incidence of morphological and genetic birth defects (3). The incidence of selected developmental defects in singleton and twin pregnancies in the Czech Republic for the period 1998-2015 is shown in Graph 6. Screening for major aneuploidy, including preeclampsia and other pregnancy risks, is inaccurate in twins and insufficient for clinical use (19).
Based on current evidence, including data from our national registry, after the reduction of twins, the pregnant woman should have the opportunity to know whether the preserved fetus, which continues to develop in the uterus, carries any serious disease that can be diagnosed prenatally by commonly available methods.
Mark Evans, who has published probably the largest sets of data of women with reduced pregnancies (10), suggests performing a chorionic biopsy before MFR and deciding on the method of MFR based on the result. We do not select the fetus for reduction due to its origin or sex (which is ethically problematic and illegal in Europe). To choose the most reliable and safe diagnostic method, we favor amniocentesis over chorionic biopsy. At CFM, after MFR, we invite pregnant women to provide an amniotic fluid sample in the 16th week of gestation analyzed by quantitative fluorescent PCR (QF-PCR) and, in case of a normal finding, by microarray examination. Our procedure is also supported by the fact that taking a sample of 20 ml of amniotic fluid according to standardized procedures no longer increases the risks for pregnancy (20).
Until 2017, we performed classic karyotyping, for which we always obtained normal results (statistically for low numbers, not evaluable from the point of view of the incidence of large aneuploidies and large chromosomal rearrangements). Since 2017, we have routinely performed QF-PCR for deviations in the number of chromosomes (13, 18, 21, X and Y). In the case of a normal finding, we used a CGH array (CGH - comparative genomic hybridization). In 3 out of 95 cases (3.2%), we detected genetic changes of significant importance. Microduplication was observed on the 1st chromosome, where a familial burden was found upon closer examination: 2 relatives with schizophrenia and delayed psychomotor development with autosomal dominant inheritance. We also detected microdeletion syndrome on chromosome 15 and the gonosomal numerical aberration XYY (also referred to as 47,XYY syndrome). Although this was a small set of data, we believe that these findings provide at least a reason to continue with this approach. In a broader context, the change in indications for the examination of amniotic fluid in twin pregnancy is increasingly discussed, since the possibilities of prenatal diagnosis have significantly advanced from the simple detection of large aneuploidies.
Multifetal reduction is an alternative method for the management of multiple pregnancy. The decision to reduce the number of fetuses should be based on individual circumstances and should be made after a nondirective counseling by an experienced specialist. This is a complex and emotionally demanding decision that should only be made after careful consideration. The supporting factors of multifetal reduction are better perinatal results for the remaining fetus (reduced risk of premature birth, growth restriction, and stillbirth), reduced health risks for the mother (reduced risk of preeclampsia and gestational diabetes) and a less physically and psychologically demanding course of pregnancy. The exclusion of chromosomal abnormalities by currently available methods in the remaining twin should be part of the management of these pregnancies.
Supported by the Ministry of Health of the Czech Republic – RVO-VFN 64165.