










 Official publication of the Czech Society of Ultrasound in Obstetrics and Gynecology.
Official publication of the Czech Society of Ultrasound in Obstetrics and Gynecology.

Introduction: Fetal MRI is increasingly being utilized as an auxiliary to ultrasonography (USG) in prenatal diagnosis. The purpose of this study was to assess how well MRI and ultrasonography agreed in patients of ventriculomegaly.
Material and Methods: This study was done retrospectively cross-sectional, and patients with ventriculomegaly detected by ultrasonography from the Koru Hospital in Ankara, Turkey, were included between January 1st, 2018, and January 1st, 2020. Patients who had isolated ventriculomegaly diagnosed on ultrasonography and afterwards underwent MRI were included. All cases were divided into three categories: mild, moderate, and severe. The ultrasound and MRI values were subsequently compared.
Results: Only included 47 fetal MRIs of patients with isolated ventriculomegaly and normal chromosomes in our study. There were 33 patients with mild (70.2%) and 14 patients with moderate (29.7%) ultrasonography findings. 34 patients (72.2%) had bilateral ventriculomegaly, and 13 (27.6%) had unilateral ventriculomegaly. However, MR imaging revealed that thirty-one (65.9%) of the patients had ventricular dilatation of 10-12 mm (mild), fifteen (31.9%) had dilation of 12.1-15 mm (moderate), and only one (2.1%) had dilation of more than 15 mm (severe). Furthermore, MRI was helpful in detecting abnormalities, particularly cortical development, which are not detected by ultrasonography.
Conclusion: MR imaging remains a priority, particularly in the prenatal identification of central nervous system abnormalities. In circumstances when ultrasound results are limited, we believe that MRI should be performed for ventriculomegaly categorization and patient prognosis.
Magnetic resonance imaging (MRI) is beginning to replace fetal ultrasonography (USG) as the main imaging modality in the assessment of prenatal abnormalities. When ultrasonography finds or predicts an issue, MRI is used (1). MRI provides improved tissue visibility with no artifacts caused by surrounding skull ossification, which is especially relevant during the third trimester when an ossified skull may limit ultrasound precision (2). Fetal MRI is a third-level diagnostic tool for the identification, assessment, and exclusion of fetal systems pathologies and represents about 80% of total MRI fetal examinations (1,2).
Ventriculomegaly (VM) is the most frequent CNS abnormality, characterized by ventricular atrial enlargement > 10 mm (3-9). VM is typically characterized according to the degree of ventricular dilatation as mild (10.0-11.9 mm), moderate (12.0-14.9 mm), or severe (15.0 mm) of dilatation being related with an increased risk of neurodevelopmental delay (10). Lateral ventricle asymmetry was defined as a difference of > 2 mm between the two lateral ventricles (10). A discrepancy of more than 2 mm between the two lateral ventricles was characterized as lateral ventricle asymmetry (10). Limitations such as maternal obesity, oligohydramnios, or incorrect fetal posture are relevant during ultrasonography because uncertainty in interpretation might arise, especially at borderline ventricular sizes. In these cases, the MRI method is used to solve problems. Measuring ventricules is significant because the degree of ventriculomegaly is connected with poor outcomes in terms of both mortality and morbidity, and it helps to provide correct information to patients when making decisions regarding the pregnancy’s future. The occurrence of significant extra abnormalities found by MRI in fetuses with mild or moderate ventriculomegaly has been reported to range between 1 and 14% (11), and potentially influence prognosis counselling.
It is a non-invasive diagnostic method that has no negative side effects. Concerning MRI safety, the American College of Radiology (ACR) has agreed that MRI examinations should be undertaken in circumstances when it is deemed to be helpful to the patient in terms of profit and loss (12). Because of its high cost, limited availability, and unproven greater diagnosis accuracy as compared to sonography, MRI is contentious (12,13).
This study was designed retrospectively cross-sectional for women who received fetal MRI after being diagnosed with ventriculomegaly through ultrasonography between January 1st, 2018, and January 1st, 2020. The study was carried out at the Koru Ankara Hospital. Ultrasound screening was done between weeks 18 and 22 of pregnancy.
Inclusion criteria: Singleton pregnancies with normal karyotype determined after delivery or amniocentesis, with normal serological evaluation of TORCH, who are determined isolated ventriculomegaly and which is why is performed an MRI. The study comprised pregnancies who had fetal MRI images between 21 and 30 weeks of gestation. Concomitant ventriculomegaly with other abnormalities, fetal chromosomal disorders, multiple pregnancies, and TORCH positive pregnancies were exclusion criteria. Patients who were diagnosed with ventriculomegaly but had no MRI or ultrasound abnormalities were excluded from the research.
Ventriculomegaly is classified as mild (10.0-11.9 mm), moderate (12.0-14.9 mm), or severe (15.0 mm). All 47 cases were divided into three categories (mild, moderate, and severe). Following that, the measures in USG and MR imaging were compared, and it was determined if the patient groups were compatible with each other using both ultrasonography and MR imaging.
Obstetricians performed the transabdominal ultrasonographic examination in accordance with ISUOG guidelines (14,15).
Measurements: Voluson E6 and E8 machines were used for the examinations, which used a 4-8 MHz volumetric convex transducer (for abdominal approach in fetuses with breech presentation) or a 6-12 MHz volumetric convex transducer (for transvaginal approach in fetuses with vertex presentation). Fetal MR imaging was performed by using a 1.5T system. Examination was performed by using T1-weighted spin-echo (SE), spectral presaturation inversion recovery, fat-saturated sequences (697/14/2; a = 90; 256 • 256; field of view (FOV), 32 cm; section thickness, 4 mm; acquisition time, 2 minutes 56 seconds; 15 sections), and T2-weighted single-shot turbo SE imaging (24 617/100/1; a = 90; 256 • 256; FOV, 280 cm; section thickness, 3 mm; acquisition time, 24 seconds).
Between the first of January 2018 and the first of January 2020, 224 ventriculomegalies were detected using ultrasonography. Only 47 fetal MRIs with isolated ventriculomegaly were included among the 97 patients that underwent MRI.
The mean maternal age was 31 (range: 27-40 SD3.84). The mean gestational age was 27 weeks (range: 22-30 SD 5). TORCH testing was performed on all of the patients who were chosen. Thirty-three patients were found to have mild (70.2%), while fourteen patients were found to have intermediate (29.7%) in ultrasound. Thirty-four patients (72.2%) had bilateral ventriculomegaly, whereas thirteen (29.7%) had unilateral ventriculomegaly. However, MR imaging revealed that thirty-one (65.9%) of the patients had ventricular dilatation of 10-12 mm (mild), fifteen (31.9%) had dilation of 12.1-15 mm (moderate), and only one (2.1%) had dilation of more than 15 mm (severe). On MRI, two cases previously classified as mild ventriculomegaly in ultrasonography were found to be moderate, while one case previously diagnosed as moderate was found to be severe. Thirteen (27.6%) of the patients exhibited unilateral ventriculomegaly, whereas thirty-four (72.3%) had bilateral ventriculomegaly (Tab. 1).
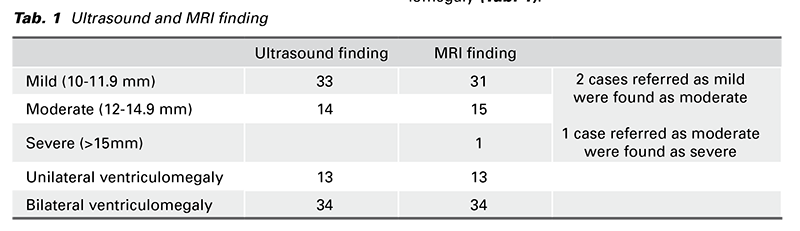
In all cases, ultrasonography and MR imaging were compatible (Fig. 1). In all cases, MRI indicated that ventriculomegaly was an isolated finding.
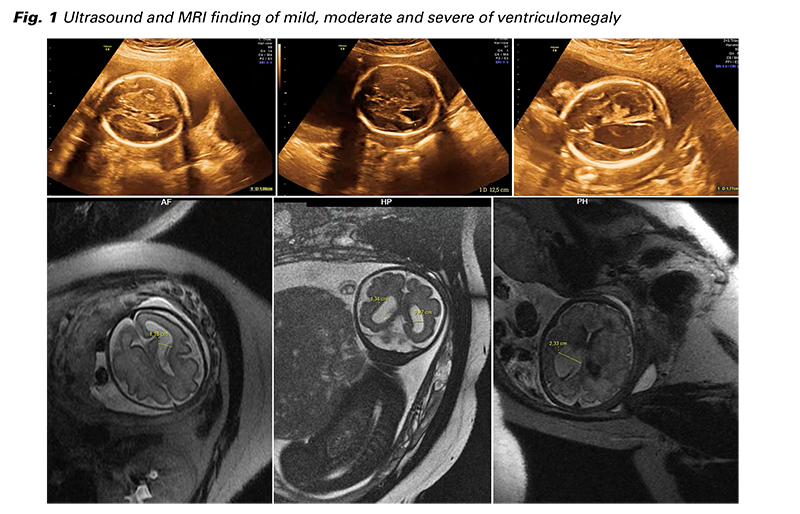
With the development of the USG method, the diagnosis of fetal abnormalities has increased in recent years. The correct diagnosis of fetal abnormalities has long been a source of contention. The mineralization of the fetal skull, complexity, maternal obesity, and differences in fetal anatomic structures all contribute to lower USG reliability. As a result, fetal MRI has been utilized to make definitive and secondary diagnoses of congenital fetal abnormalities. Fetal MRI is a third-level diagnostic technique for identifying, assessing, and ruling out fetal system pathologies, accounting for about 80% of total MRI fetal examinations (12). MRI is a non-invasive diagnostic procedure that does not use ionizing radiation and has no side effects. In terms of MRI safety, the ACR has agreed that MRI can be done on patients who are considered beneficial in terms of profit and loss. Bilateral moderate ventriculomegaly increases the risk of cerebellar maldevelopment and delayed neurological development, but isolated moderate bilateral ventriculomegaly has no consequence (16). Confirmation of ventriculomegaly degree is important because severe ventriculomegaly is associated with high risk of clinical outcomes (17). According to some research, if the ventriculomegaly is mild, infants have a 97.7% chance of survival at 24 months. In moderate ventriculomegaly, this rate is 80%, whereas in severe ventriculomegaly, it is 33.3% (18). The sequela-free neurodevelopment of surviving infants at 24 months was found to be 93%, 75%, and 62.5%, as appropriate (19). Because the prognosis is strongly connected to the degree of ventriculomegaly, it is beneficial to prefer MR imaging in cases where ultrasound imaging is limited. Prenatal precise ventriculomegaly measurement is important for proper classification and providing more accurate prognosis information to the family. Based on this information, a decision is made regarding whether to continue or terminate the pregnancy. Some studies have demonstrated that in utero MRI is more accurate than USG for detecting CNS abnormalities (19-22). However, there are studies that show the opposite of this view (23). In our study, we compared ultrasonography findings of ventriculomegaly to MRI. Consequently, two mild cases were determined to be moderate, and one moderate case was determined to be severe in MRI. Our study showed that MRI and ultrasound measurements are substantially compatible. On MRI, the same results were verified in 13 referred patients with unilateral ventriculomegaly and 34 patients with bilateral ventriculomegaly. MRI indicated that ventriculomegaly was an isolated finding in all cases. Based on these findings, we concluded that USG is adequate for measuring the ventricle. However, we believe that MR imaging might be more accurate, depending on the conditions that limit ultrasonography (24) (especially calvarial ossification and fetal position). Because MR imaging offers higher contrast resolution and is less affected by maternal body habitus. The severity of ventricular dilatation affects the prognosis. As a result, we place tremendous emphasis on ventriculomegaly categorization. The inadequacy of our study is that it is retrospective, and we did not eliminate the bias of referral to MR imaging. For example, it is possible that fetomaternal specialists may have referred patients with ventriculomegaly to MR imaging because they thought that ventriculomegaly was accompanied by other central nervous system anomalies, except for restrictive conditions.
When this modality and professional radiologic interpretation are available, we recommend that MRI be used in situations of a mild or moderate fetal ventriculomegaly. The value of the MRI would be reduced if a comprehensive ultrasound was conducted by someone with particular training and competence in sonographic imaging of the patient’s fetal brain. We believe that MRI is important in assessing prognosis in intermediate cases.
All authors have reviewed and accepted its submission of the manuscript and the manuscript has not been published and is not being considered for publication anywhere in whole or in part in any language. This study was completed in line with the Helsinki Declaration. There is no competing interest. The study protocol was approved by the Ethical Committee of Yuksek Ihtisas University. (E 2022/14/04)